Our website is not supported on this browser
The browser you are using (Internet Explorer) cannot display our content.
Please come back on a more recent browser to have the best experience possible
MIGSO-PCUBED were engaged to support an NHS hospital trust in implementing a digital dictation software tool that enabled medical speech recognition application for clinical staff.
The trust had purchased the software but had no capability to engage teams, drive the adoption and release the short and long term benefits of the solution. The scope of this project revolved around change management services to transform ways of working for clinicians, nurses and admin staff at the trust. This would result in quicker digitised work processes allowing administrative and secretarial staff to focus on activities with greater added value for patients.
There were a number of reasons for slow adoption, including:
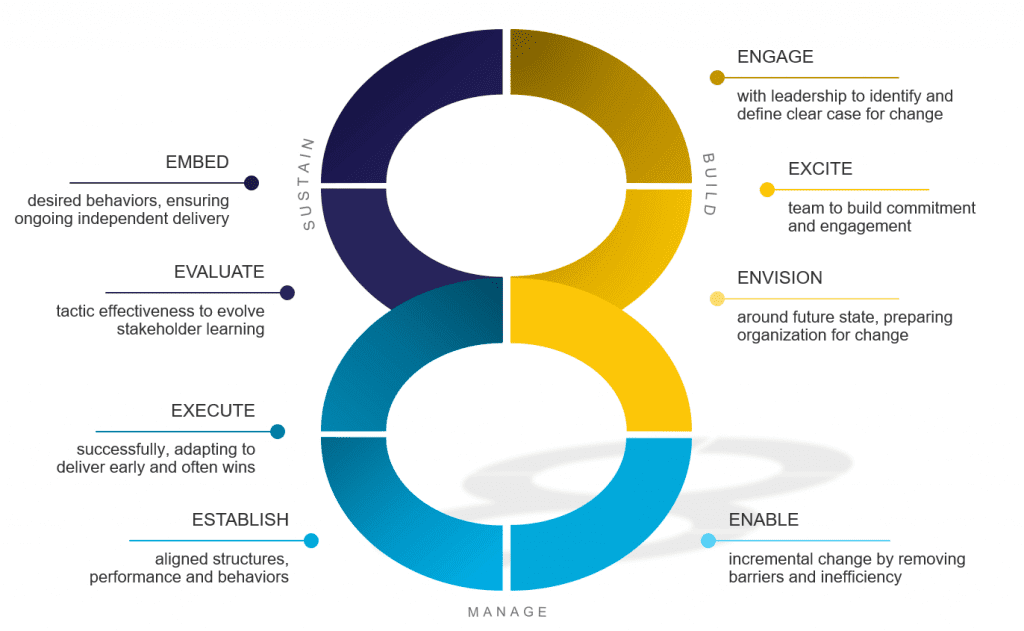
An M|P team used our 8E change management approach that is aligned to an industry recognised ADKAR change management methodology, developed by PROSCI. The image below helps to explain our 8E approach which is centered around driving ‘adoption’. Until the change is embedded and the desired outcomes are delivered, it would not be possible for the Trust to fully realise the benefits of using the tool. The 8E approach supports a change initiative throughout the traditional project phases; from identifying and defining the change, to delivering the initiative, and to finally close the initiative.
The below outlines some of our key change management learnings from our experience working with clinical teams in supporting them to make changes to their ways of working:
One of the first things the MP team set out to do was define the benefits of the implementation and create the case for change. MP defined a set of benefits metrics for the software that measured the usage of the new tool and were both quantifiable and measurable. The proposed benefits were baselined and adoption levels were set with key stakeholders.
Knowing and being able to articulate the quantifiable and measurable benefits of adoption helped to create a clear message around why this change was happening. It was used within communications to help people understand the benefits and financial gains of the change in ways of working; a big motivator for some.
Once the anticipated adoption levels and the baseline were known, financial benefits of using this tool were quantified and the impact for individuals and teams across the whole trust were understood.
MP used adoption data to create automated visual dashboards that could be shared across the trust to track adoption progress and create a healthy sense of competition between departments.
A critical component of any change is having a robust network of change agents that can facilitate stakeholder engagement, communications and role model the change.
MP established a community of “superusers” for the new software, creating a network of superusers that spanned across all departments of the trust and acted as the champions of the change.
Superusers are those who used the tool in their day-to-day activities, acting as early adopters with a unique opportunity to innovate and identify ways that will help their colleagues get the most out of the tool. Supported by MP guidance the super users were instrumental in engaging recipients of the change to train, communicate and onboard them and their colleagues. This network was also key in creating tailored training and support materials for the product.

With the help of the superuser community, MP was able to run a number focused pilots across the trust. In these small pilot areas, all clinicians adopted the tool, and the benefits of using it could be clearly and visibly demonstrated. Communicating and sharing these early wins is essential as it provides early validation of the changes and helps to build momentum with change efforts. Providing this feedback to leadership/sponsors will help to promote their vision for the tool, and galvanize the wider community to support those working hard on adopting the new ways of working, helping to attract those who are not actively adopting or onboard with the change.
During previous attempts of implementing other dictation software, clinical teams had received no comprehensive training or support in using the tools. Clinical teams in the NHS were already at capacity and overstretched. Support was required to develop the skills the recipients of the change needed to adopt the new tool.
The MP team used the superuser community to understand the training requirements and create a plan to upskill teams to help accelerate their adoption of the tool. The learning was delivered across a variety of accessible formal and informal formats. The most effective way of getting clinicians onboard and upskilled in the tool were running face– to– face sessions within the local clinical setting, where a super user could demonstrate the tool and give users an opportunity to put it into practice.

As a result of MP engagement, the trusts software license allocation increased from 29% to 75% during 3 months and usage of these licenses was more than doubled. The advanced user community grew from 90 users to over 240 users and all departments across the trust had an embedded superuser who was known and able to continue to support their area in making the sustained changes after MP departed.
In some pilot scenarios the impact of the dictation tool allowed direct reductions in the patient letter backlog. In some instances turn around times for patients waiting to receive their letters reduced from 6 weeks to just 48 hours.
This article was written by: Alice Evans, Delivery Manager
Loved what you just read?
Let's stay in touch.
No spam, only great things to read in our newsletter.
We combine our expertise with a fine knowledge of the industry to deliver high-value project management services.
MIGSO-PCUBED is part of the ALTEN group.
Find us around the world
Australia – Canada – France – Germany – Italy – Mexico – Portugal – Romania – South East Asia – Spain – Switzerland – United Kingdom – United States
© 2024 MIGSO-PCUBED. All rights reserved | Legal information | Privacy Policy | Cookie Settings | Intranet
Perfect jobs also result from great environments : the team, its culture and energy.
So tell us more about you : who you are, your project, your ambitions,
and let’s find your next step together.
Dear candidates, please note that you will only be contacted via email from the following domain: migso-pcubed.com. Please remain vigilant and ensure that you interact exclusively with our official websites. The MIGSO-PCUBED Team
Choose your language
Our website is not supported on this browser
The browser you are using (Internet Explorer) cannot display our content.
Please come back on a more recent browser to have the best experience possible